To select a COBRA Open Enrollment service with us (Ameriflex) that best suits your needs, please complete the following steps:
1. Log in to the Ameriflex Portal.
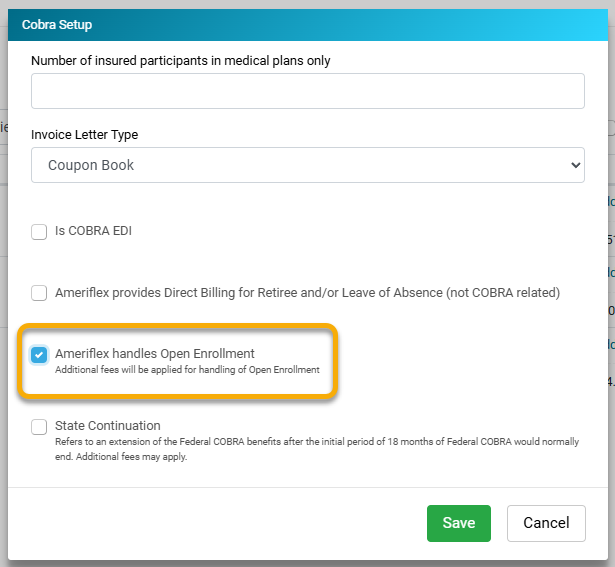
2. Check the box that states Ameriflex handles Open Enrollment during the COBRA setup step of the renewal process.
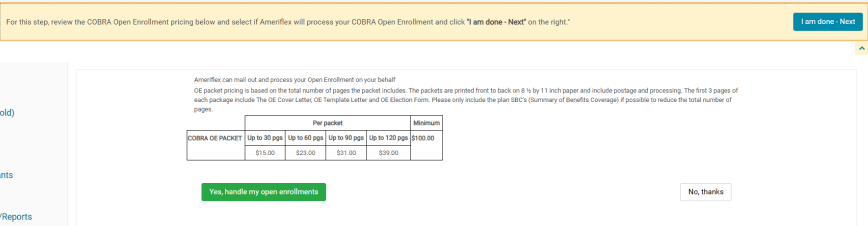
3. In the guidance panel, click the Go to COBRA open enrollment service agreement to review and agree to the additional service add-on.
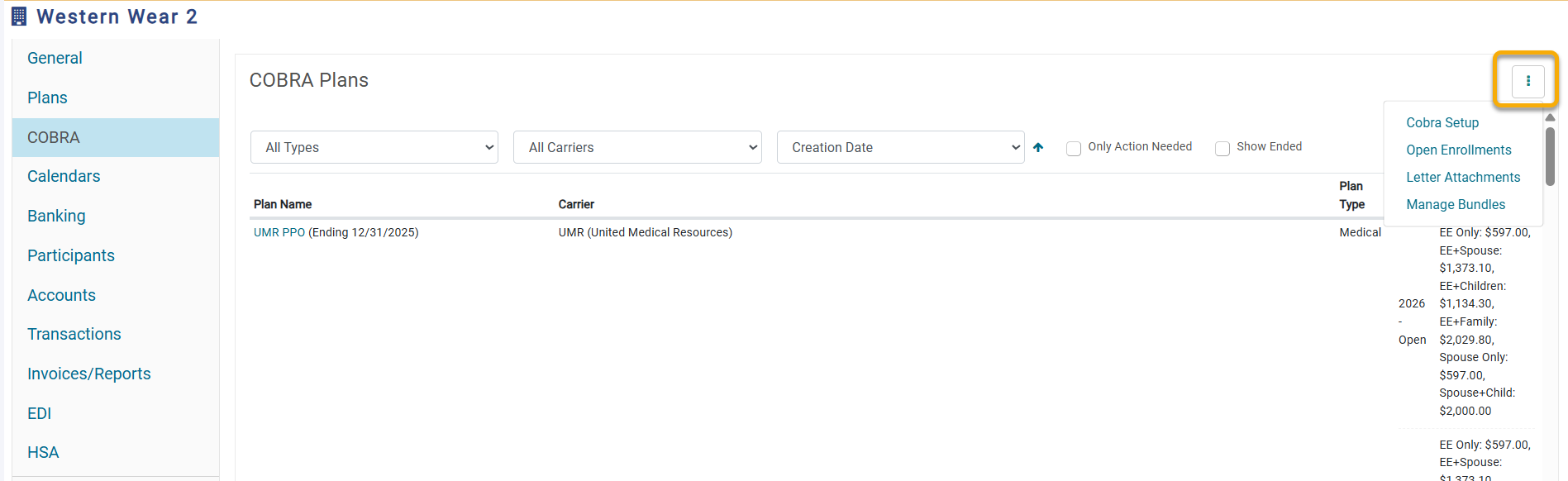
4. Click on the COBRA tab on the left-hand side of the screen.
5. Click the three vertical dots (⋮) in the top-right corner.
_in_the_top-right_corner..png)
6. Select Open Enrollments.
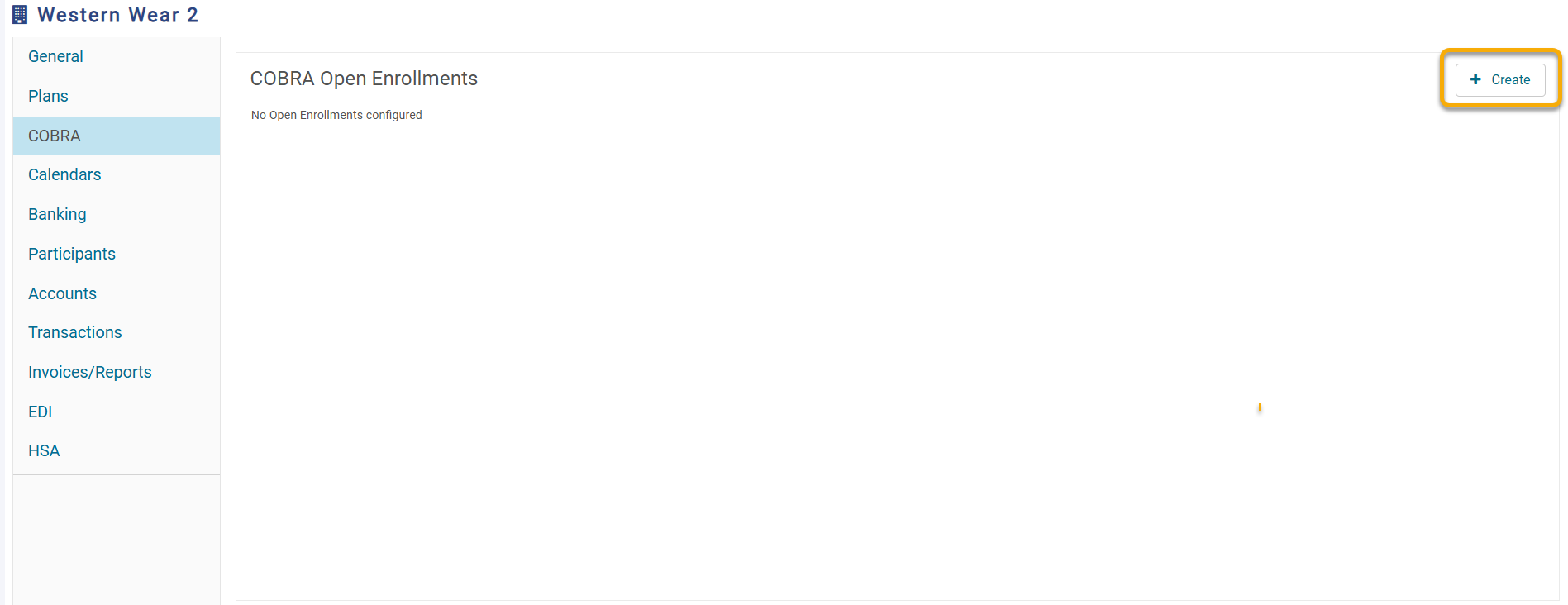
7. Click the + Create button in the top-right corner.
8. The new Create Open Enrollment screen will appear.
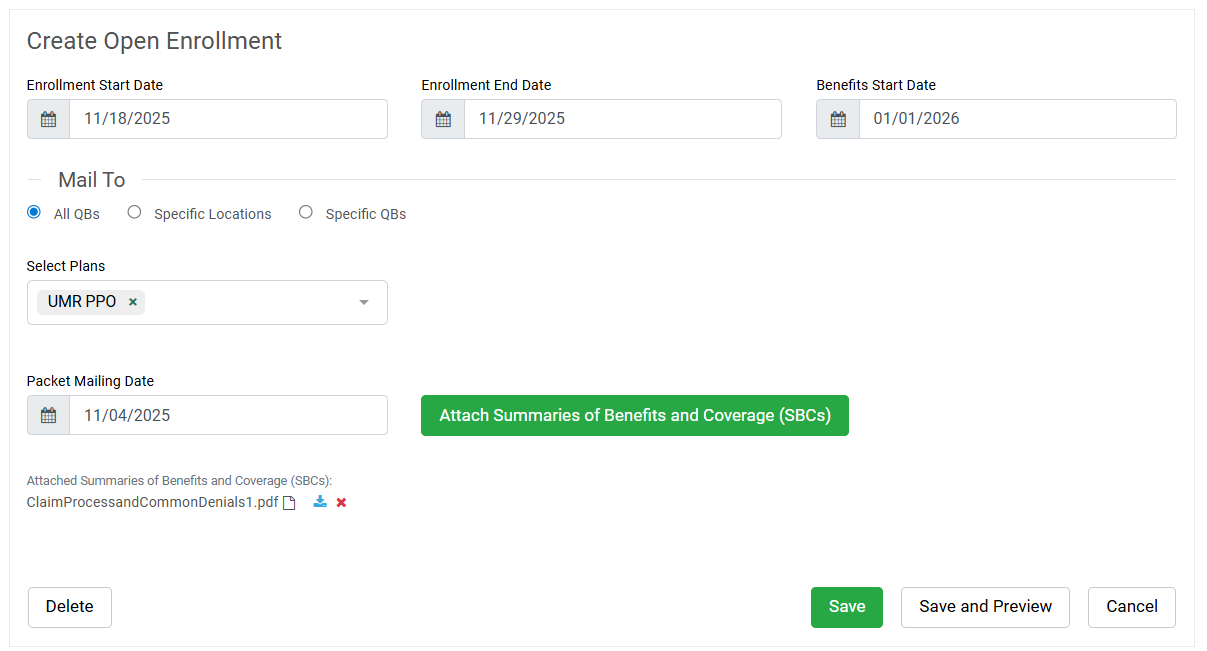
Here you will be able to configure:
- Enrollment Start and End Date - this will be the dates that a Qualified Beneficiary (QB) has to make changes.
- Benefits Start Date - this will be the date the new benefits start.
- Mail To: - this will be who Ameriflex will be mailing Open Enrollment Packets to. You can choose from the following options:
- All QBs
- Specific Locations - this would be for groups that have multiple locations and would like the packet sent to only QBs in a particular location.
- Specific QBs - this will change the Save button on the bottom of the page into a Next button so the employer/broker can manually select QBs or upload a spreadsheet.
- Plans - here you will be able to select the plans that are in open enrollment so the QB can make their changes if desired.
- Packet Mailing Date - this will be the date you would like the packets mailed out by.
- Attached Summaries of Benefits and Coverage (SBCs) - here you will be able to upload the SBCs for the QBs to review.
- The Rate sheet will be automatically generated. If they are banded rates, we will upload a page that lays out the rates.
- Please note that this cannot be edited. If the group would like a custom sheet, please upload a separate page under the Attached Summaries of Benefits and Coverage (SBCs) section.
9. Once completed, you will be able to select Save. Here you will be provided the Cost Estimate per Packet.
10. If you approve, you can then select Continue. You will now see the link to your COBRA Open Enrollment packet information.