Complete the following steps to see the benefit termination type of a plan:
1. Log into the Ameriflex Client Portal.
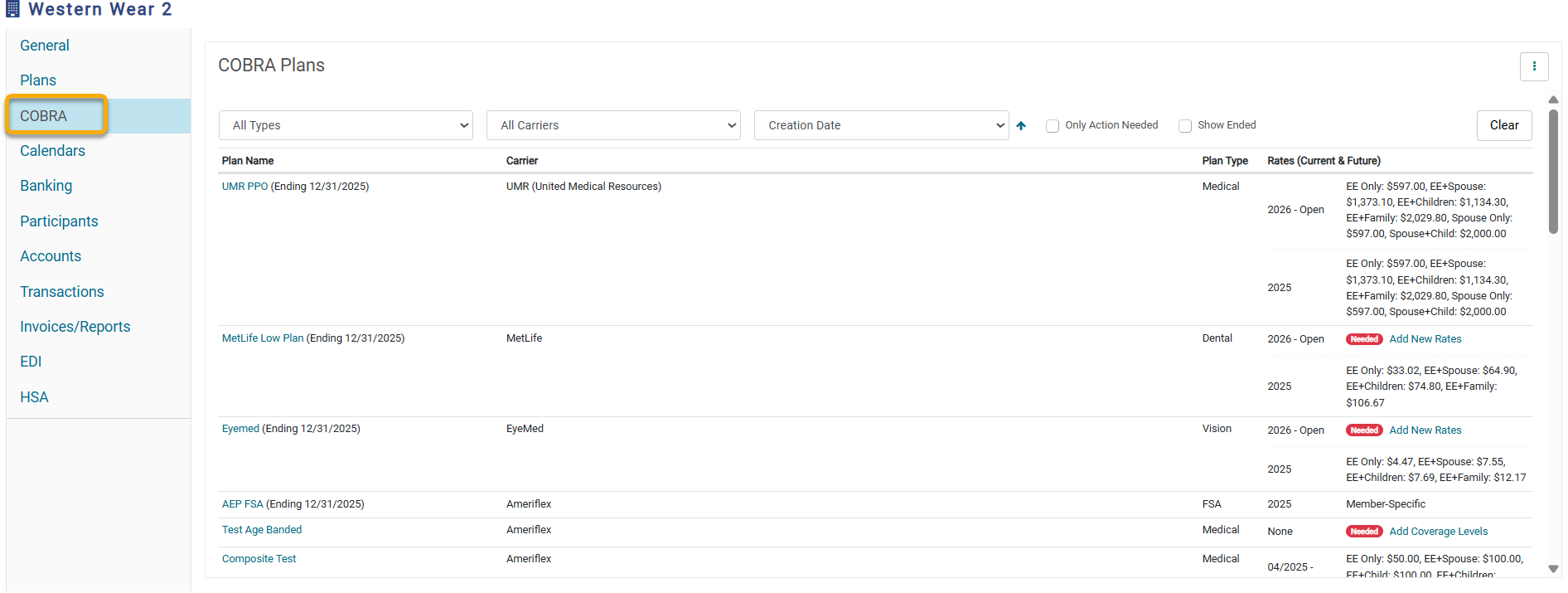
2. Locate and select the COBRA tab from the menu to the left of the page.
.png)
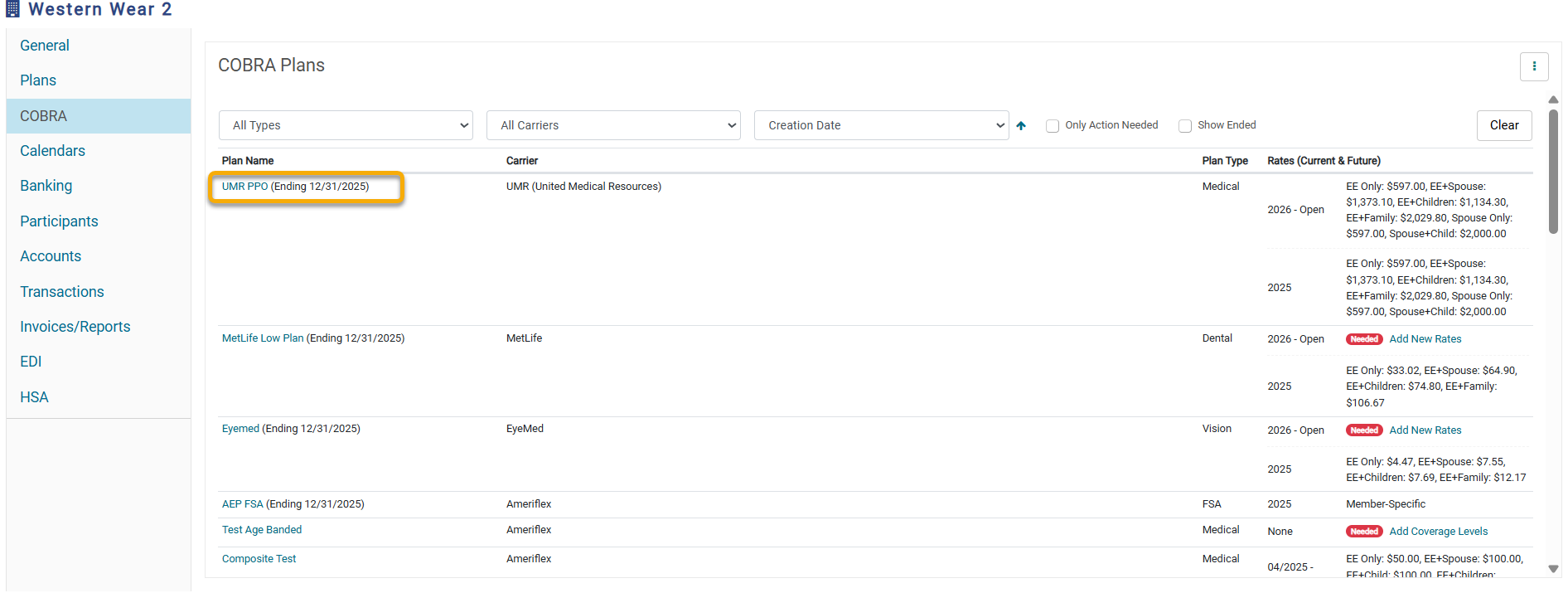
3. Once the COBRA Plan page appears, select the blue Plan Name hyperlink. The plan details will appear.
.png)
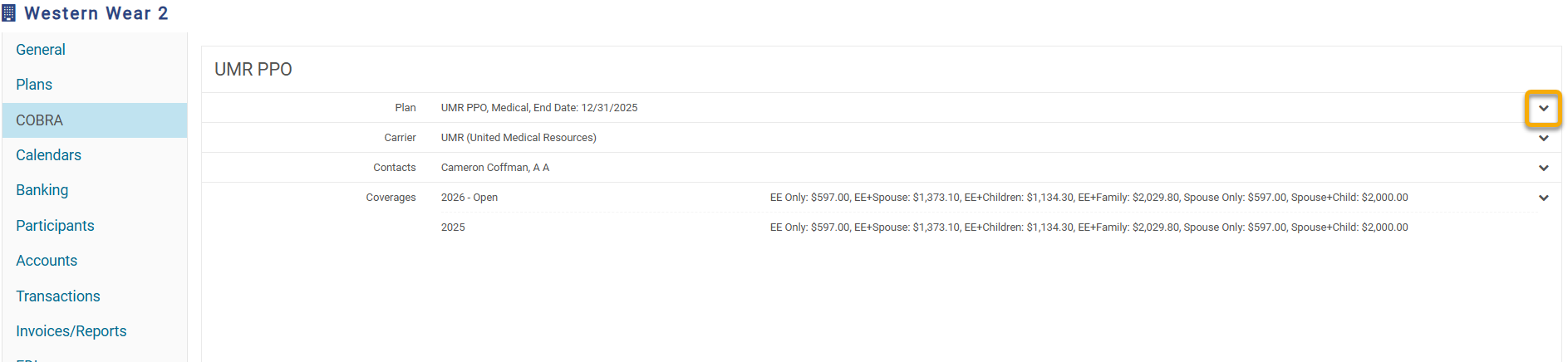
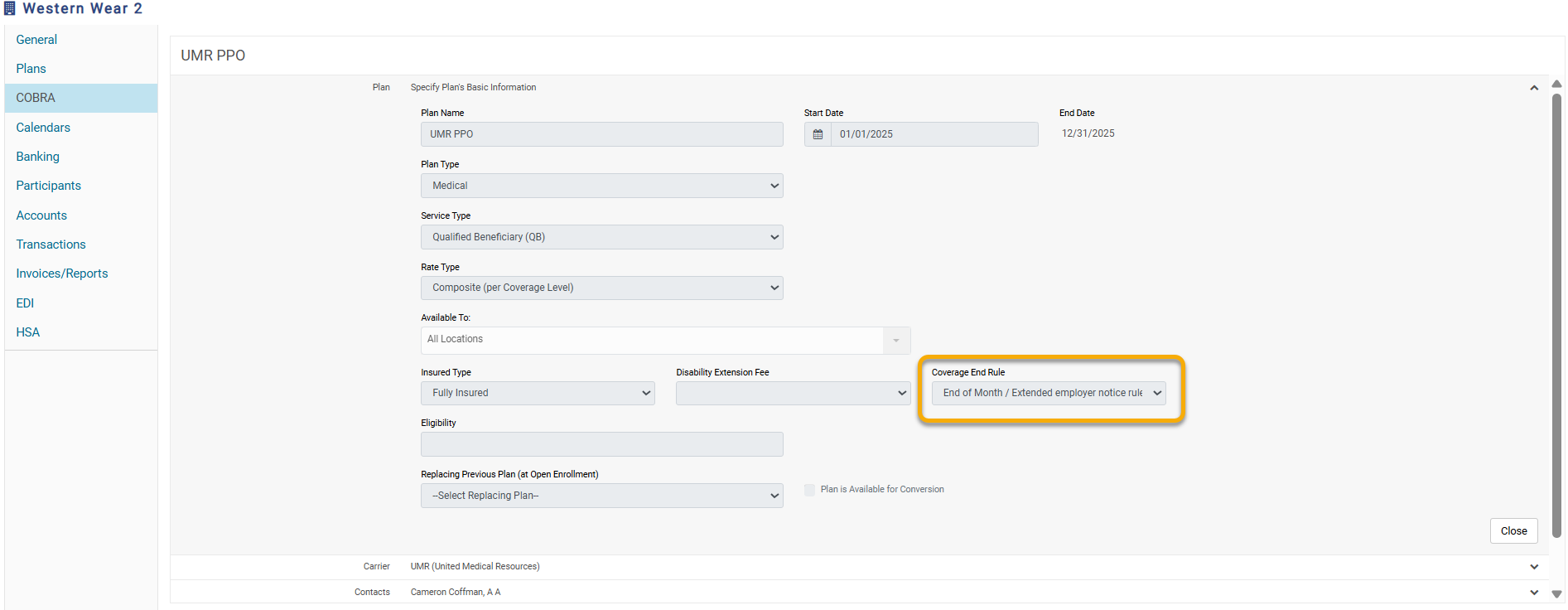
4. Select the drop-down arrow next to the Plan section to expand the details.
The benefit termination type will show under the Coverage End Rule field.
.png)
Date of Qualifying Event - Employees' coverage with the group will terminate on the date of the qualifying event. COBRA coverage will start the following day. For example, if the employee termed on 04/25/2025, COBRA will begin on 4/26/2025.
End of Month/Extended Employer Notice Rule - Employees will have coverage with the group until the end of the month they are termed in. COBRA coverage will begin on the 1st of the following month. For example, if the employee termed on 4/25/2025, COBRA starts on 05/01/2025.
Employer Notice Rule (also known as Wash/Roll Rule) - If an employee is termed between the 1st and 15th, their COBRA coverage will start the following day. If they are termed between the 16th and 31st, their COBRA coverage will start on the 1st of the following month. For example, if the employee termed on 4/12/2025, COBRA will start on 4/13/2025; if the employee termed on 4/25/2025, COBRA will start on 5/1/2025.