If you use your Ameriflex Debit Mastercard, MyPlanConnect automatically tries to locate the Explanation of Benefits (EOB) for your transaction. When MyPlanConnect finds the EOB, you'll be all set and no further documentation is required.
If you pay out-of-pocket for a transaction, MyPlanConnect allows you to easily submit the claim.
Continue reading to learn how to set up MyPlanConnect and use it.
How to Set Up MyPlanConnect
1. Log into your Ameriflex account
2. Locate and select the More tab at the top of the page.
A dropdown menu appears.
3. Select MyPlanConnect from the list of options.
4. Click Manage Carrier Connections.
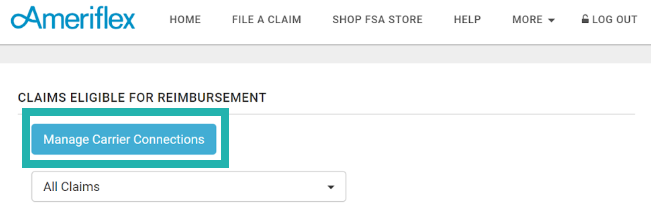
The New Plan Connection page appears.
5. Click the dropdown arrow to review and select your healthcare provider.
6. Fill out your healthcare provider username and password.
7. Click into the box next to 'I agree to the terms and conditions' text to confirm you agree.
8. Click Save connection.
The 'Your Dependents' page appears with a list of your dependents, if you have any.
9. Click the +Invite button next to each dependent's name to send them a link to connect their carrier connection.
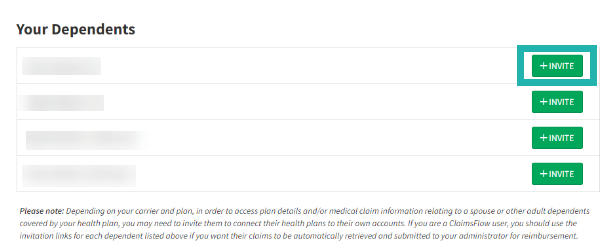
You successfully set up your MyPlanConnect.
Navigating MyPlanConnect to Submit a Reimbursement
1. From your Ameriflex account, view list of EOBs on the Home Page.
2. Hover over and select an EOB to view that specific EOB's claim details.
The Claims Details page for that specific EOB appears.
3. Under the Eligible for Reimbursement section, locate the Account Type field and click the dropdown arrow to select which account to reimburse the claim.
A window prompt appears.
4. Select Pay Myself or Pay Provider.
5. Complete one of the following steps based on your selection for Step 4:
- If you selected Pay Myself in Step 4, select the check box and click Submit reimbursement.
- If you selected Pay Provider in Step 4, fill out the provider's information. Then, select the check box and click Submit reimbursement.
You successfully navigated MyPlanConnect to submit a reimbursement.
Additional Information
- How will participants receive a substantiation notice 90 days after if an EOB is not transferred for an expense?
First Request: The first notification is not requested immediately as the system allows the carrier 90 days to post the Explanation of Benefits. If the Explanation of Benefits has not posted after 90 days, Ameriflex will send out the first notice to notify the member that we will require the proper documentation since it did not post within the system.
Second Request: If the participant does not respond to the 1st request and/or the EOB never loads from the carrier site, a second request will be sent. If the second request is nor responded to, or if we receive incomplete documentation, the transaction may cause the plan to be deactivated until the transaction is cleared. Ax Explanation of Benefits is best to substantiate claims, especially for HRA accounts, however non HRA accounts can also accept itemized receipts. Itemized receipts need to include the date of service, services rendered, amount charged and name of the provider.
Ineligible or Insufficient: Transaction will be labeled ineligible if proof is received that deems a transaction is not eligible or if insufficient documentation has been received.
- How do I troubleshoot if I get disconnected?
You may get disconnected from your carrier if you reset your password on the carrier site or if there is an error with the connection. We recommend checking your connection every so often to ensure you are still connected. You can check this under the MyPlanConnect page within the Employee Portal.
- If I change my healthcare provider username and password, how do I update the MPC connection?
When your employees change their username and password on their insurance carriers member portal, they will also need to update this information on our portal so that their carrier continues to provide the employee’s Explanation of Benefits (EOBs) to Ameriflex’s participant portal site. Once on MyPlanConnect, navigate to the “Health Plan Connections” section. Select “Re- Enter Username/ Password” to enter new information.