If we receive a COBRA benefits appeal letter requesting benefits be reinstated, we will first reach out to notify you.
Ameriflex must respond to the participant within 30 days from the date of the appeal letter, so upon receipt, please let us know if you would like to approve or deny the appeal.
You have two courses of action: to approve or deny the appeal.
To approve the appeal, please complete the COBRA Plan Administrator Override Form and return it to us for processing via our secure portal.
To upload documents:
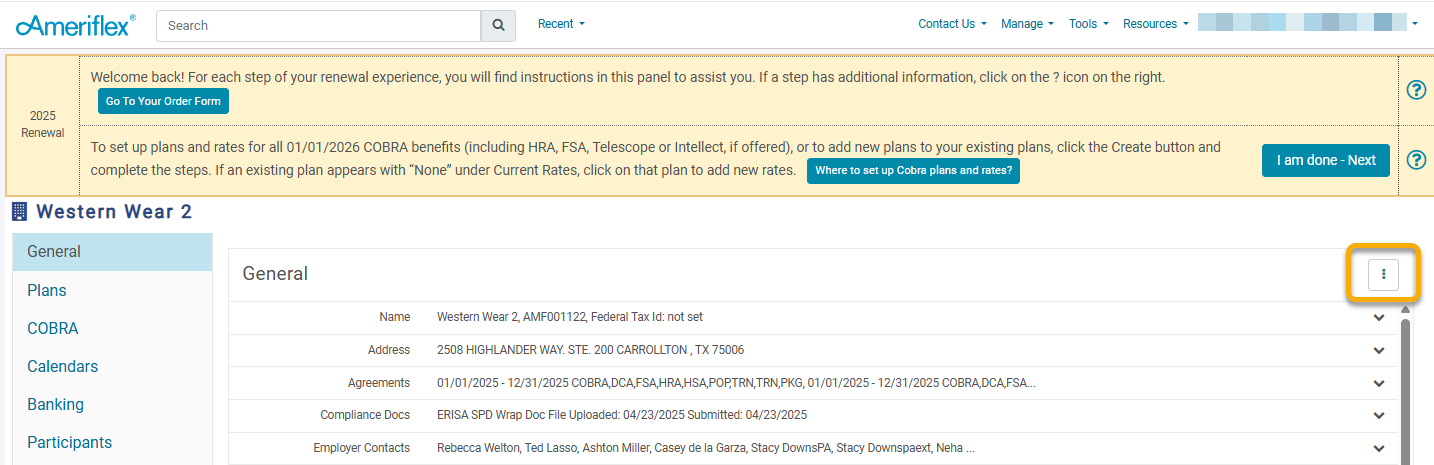
1. Log into the Ameriflex Employer portal.
2. On the General tab, click the three dots (ellipsis) on the top right.
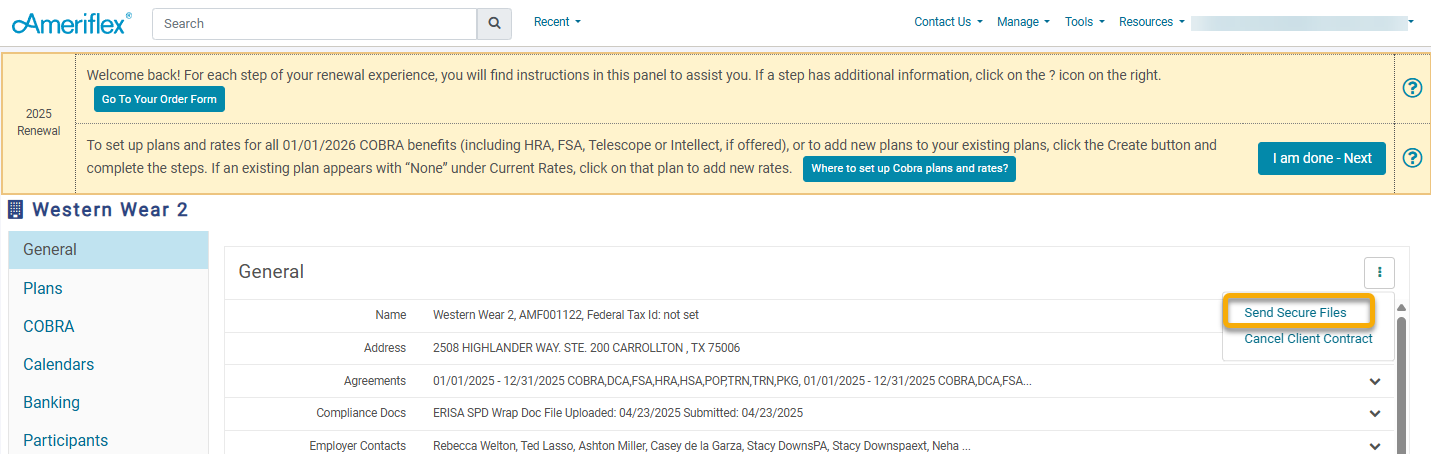
3. Once you click on the ellipsis, you’ll receive a dropdown menu. Click the Send Secure Files option.
4. You will receive a new pop up window. Use the drop down menu to select where you are sending the File, as you may be working with both a COBRA and Flex team if you have both types of plans.
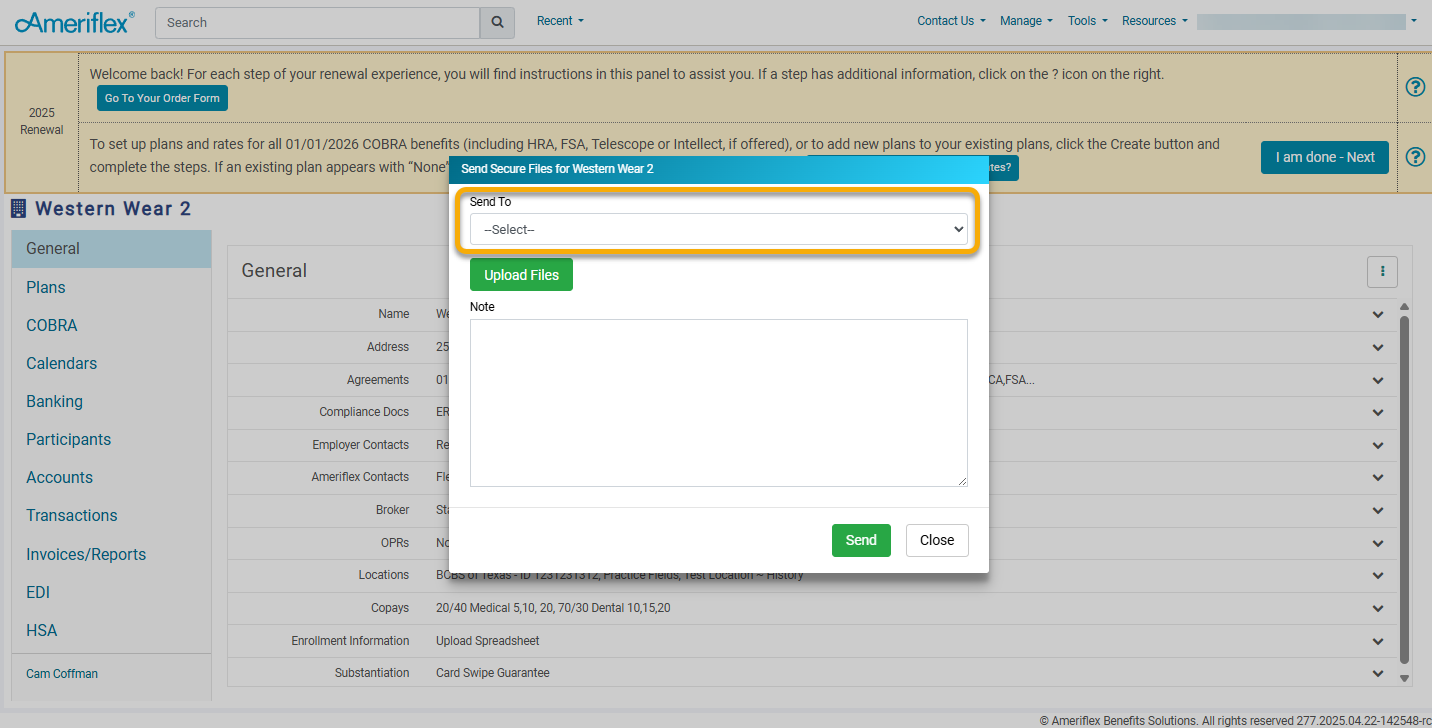
5. Once you've selected the appropriate team from the dropdown, click on the green Upload Files button to upload the File saved on your desktop. Add a Note if you need to give the receiving team additional instructions, then click on the green Send button.
In the event that you would like to deny the appeal, please confirm via email indicating that you would like to deny this appeal.
While Ameriflex typically advises against allowing late payments/reinstatements to help keep the employer in compliance with Federal COBRA regulations, we understand there are times when exceptions need to be made. Therefore, we leave this to the employer’s discretion on how they would like Ameriflex to proceed. However, it is essential to note that any decision made may set a precedent that could apply to all similar COBRA appeals.
To view your COBRA participants’ information, visit the Ameriflex Employer portal.