An Eligible Plan Member is an individual who is a current employee of an employer and is not yet receiving COBRA benefits but is on group coverage.
By following these steps, you will generate an Initial Rights Notice. You must furnish this notice letter to all active employees within 90 days of enrollment in the group health plan.
To add an Eligible Plan Member and generate the Initial Rights Notice, complete the following steps:
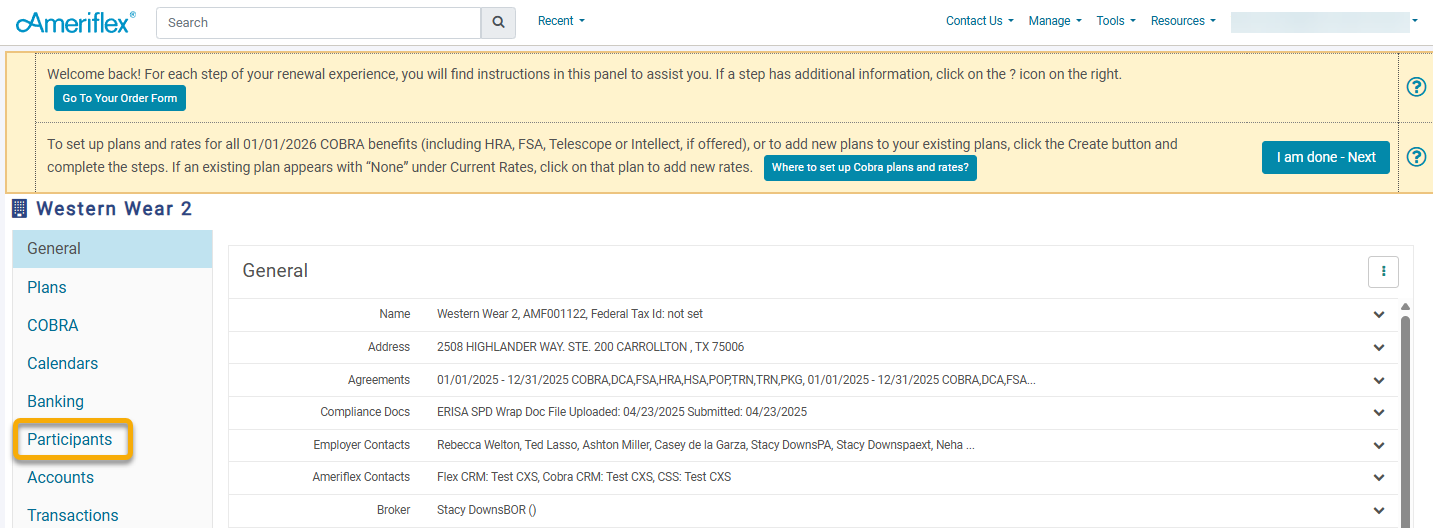
1. Log in to the Employer Portal.
2. Select the Participants tab on the left side of the page.
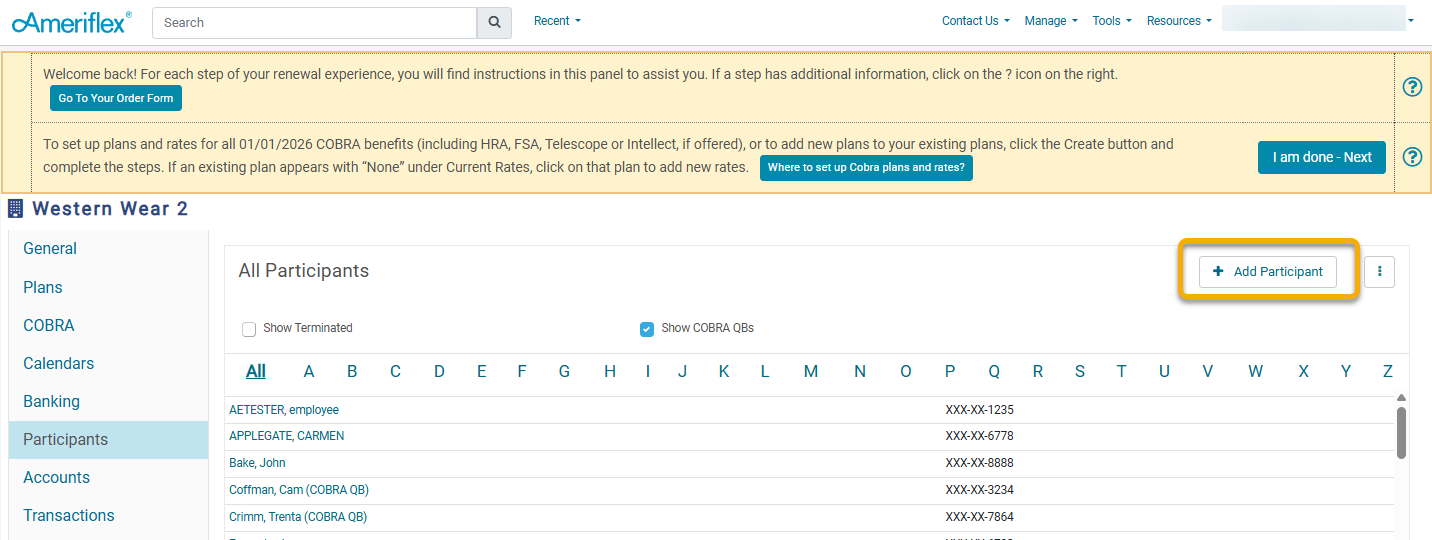
3. Select the Add Participant button in the top right corner of the Participants screen.
4. A Create Participant pop-up will appear. Fill in the contact information in the form, then check the Should Receive Initial Rights Notice box towards the bottom. Once finished, click Save.
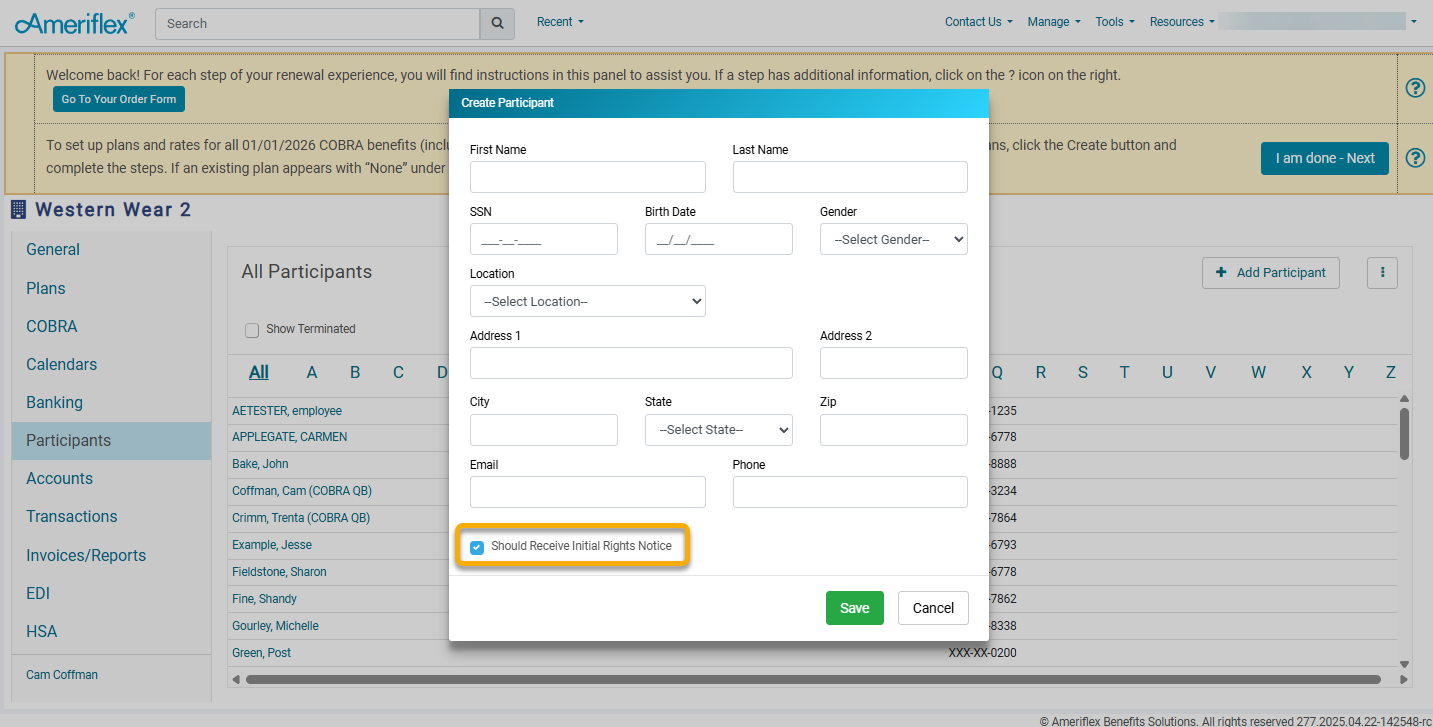
5. Click Create.